Myasthenia gravis
Find a neuro specialistMyasthenia gravis (MG) can come on suddenly, causing muscle weakness in different parts of your body. Since myasthenia gravis symptoms are like symptoms for other conditions, it may take time for you to get a confirmed diagnosis. Your Advocate Health Care doctor will collaborate with specialists to develop a personalized treatment plan that works for you and minimizes your symptoms.
What is myasthenia gravis?
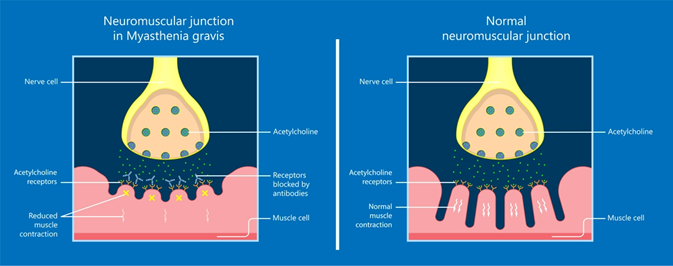
Muscle weakness is caused when messages from the brain are blocked from getting to your muscles. When you have MG, some of the chemical (acetylcholine) that carries messages from the brain can’t get to the muscles because abnormal antibodies get in the way. When that happens, your muscles don’t contract as well, and you feel weakness.
Myasthenia gravis & the thymus gland
Myasthenia gravis is also related to problems with the thymus gland, which controls the immune system during childhood. Scientists think that the thymus is involved in the growth of abnormal antibodies that block acetylcholine.
Normally, the thymus gland grows until you reach puberty and then gradually shrinks until it gets replaced by fat. In many people with myasthenia gravis, the thymus remains large and may develop tumors (thymomas). Thymomas are usually benign, but they may become cancerous. Having a thymoma or a large thymus may be a sign that you have myasthenia gravis.
Myasthenia gravis symptoms
Symptoms of myasthenia gravis vary quite a bit. For some people, it affects mainly the eyes and face. Other people have weakness in only one part of the body or all over the body. Some of the most common myasthenia gravis symptoms are:
- Weakness of the eye muscles (ocular myasthenia)
- Drooping of one or both eyelids (ptosis)
- Blurred or double vision (diplopia)
- Changes in facial expressions
- Difficulty swallowing
- Shortness of breath
- Impaired speech (dysarthria)
- Weakness in the arms, hands, fingers, legs, and neck
One of the things that makes myasthenia gravis symptoms different from symptoms of other conditions is that muscle weakness gets worse with activity and gets better after rest.
Symptoms of myasthenia gravis can be life-threatening if they affect your breathing to the point where you need a ventilator (myasthenic crisis). Seek emergency treatment or call 911 if you have extreme trouble breathing.
Triggers for myasthenia gravis symptoms
Several things may act as a trigger to make myasthenia gravis symptoms worse. Some of them are:
- Warm weather
- Surgery
- Emotional stress
- Illness such as a virus
- Pregnancy and postpartum period
- Worsening of another chronic illness
- Some medications
Myasthenia gravis risk factors
There are no known myasthenia gravis risk factors. Myasthenia gravis is more common in women younger than 40 and in men older than 60. It’s not contagious or inherited, and it affects people in all racial and ethnic groups.
Myasthenia gravis diagnosis & testing
Myasthenia gravis diagnosis can be difficult because the symptoms overlap with other conditions such as stroke, brain tumors or other neuromuscular conditions. Your doctor will perform a physical exam and ask about your symptoms and medical history. They’ll also do a neurological exam to test your coordination, sense of touch, eye movements, and muscle strength and tone.
They may order blood tests to check for specific kinds of antibodies. They may also order these tests:
- Repetitive nerve stimulation: Checks muscle responses by stimulating nerves repeatedly with electricity.
- Electromyography (EMG): Electromyography checks for problems in communication between nerves and muscles. It’s the most sensitive myasthenia gravis test.
- Computed tomography (CT) of the chest: Checks for a thymoma or enlarged thymus.
- MRI of brain and eye orbit: Looks for growths unrelated to MG that may be causing eye symptoms.
Myasthenia gravis treatment options
Treatment for myasthenia gravis focuses on treating symptoms and improving your quality of life. There’s no cure for MG, but researchers are looking for better treatments.
One option for myasthenia gravis treatment is surgical removal of the thymus gland. Research shows that removing the thymus improves myasthenia gravis symptoms and may cause remission (temporary recovery).
When it comes to myasthenia gravis medications, there are several options. Cholinesterase inhibitors cause the effects of acetylcholine to last longer and increase the chances of messages getting through to your muscles. Corticosteroid and immunosuppressant drugs may relieve MG symptoms, although side effects from corticosteroids may be a problem.
Myasthenia gravis treatments with blood products
Doctors may recommend a blood plasma exchange if a person needs to have surgery or suddenly has worsening symptoms. An apheresis machine is used to filter the plasma from the person’s blood and replace it with donated plasma. This removes the abnormal antibodies that are causing muscle weakness.
Another potential treatment for myasthenia gravis is intravenous immune globulin (IVIG) infusion. Immunoglobulins (antibodies) are separated from donated plasma from thousands of people and injected into the bloodstream of the person who has MG. Since the donated antibodies are normal, they improve muscle strength.
Both of these myasthenia gravis treatments with blood products take several hours to complete and are usually provided as outpatient procedures.
Get care
We help you live well. And we’re here for you in person and online.