Intraventricular hemorrhage
Find a neuro specialistIntraventricular hemorrhage (IVH) is a serious medical condition characterized by bleeding within the ventricles of your brain that contain spinal fluid. When bleeding occurs, it impacts brain function and may lead to long-term complications.
Call 911 or get to the nearest emergency department if you are experiencing symptoms of an intraventricular hemorrhage.
What is an intraventricular hemorrhage?
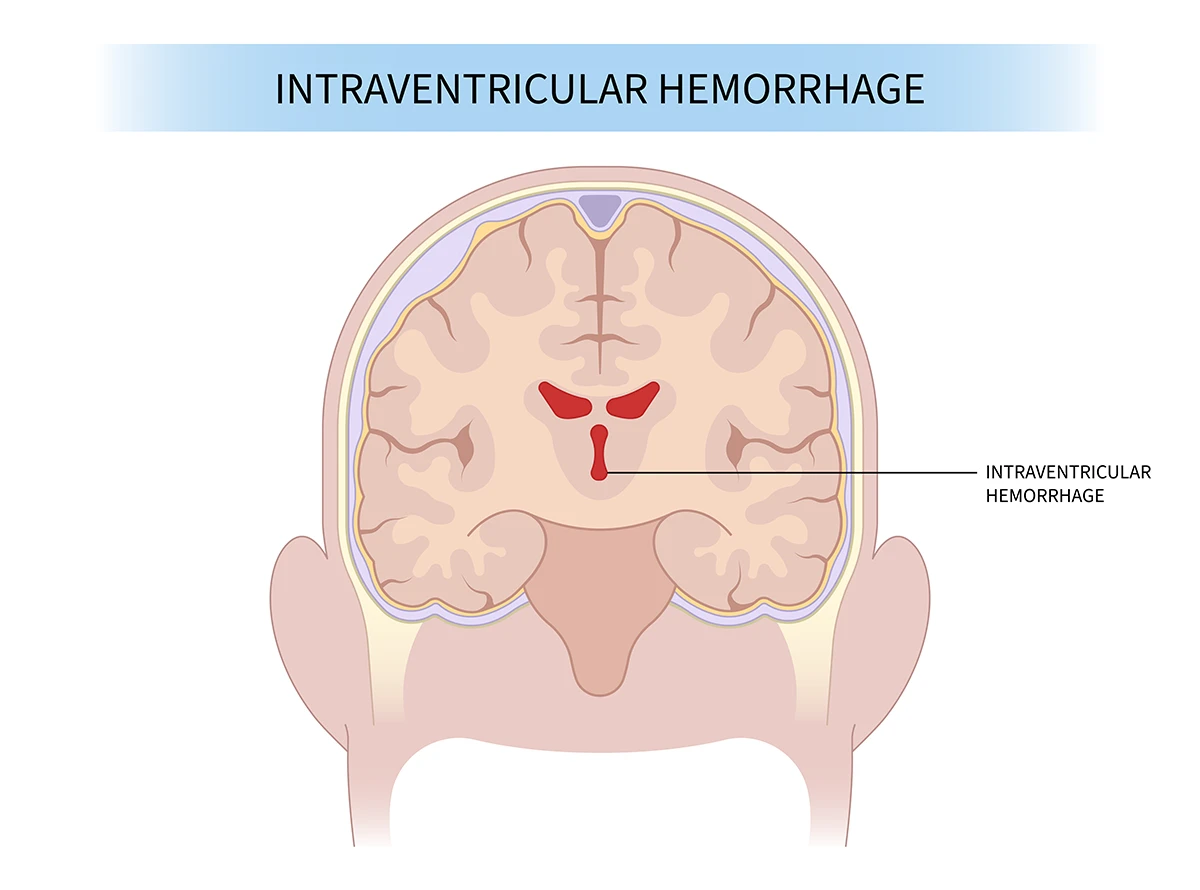
The location and size of an intraventricular hemorrhage in the brain.
An intraventricular hemorrhage is a type of brain hemorrhage where bleeding occurs within the brain's ventricular system, which is a network of fluid-filled spaces. The ventricles are responsible for producing and circulating cerebrospinal fluid (CSF), which cushions and protects the brain.
An intraventricular hemorrhage is more common in premature infants, particularly those born 32 weeks before gestation. This condition occurs when the tiny blood vessels in the fragile area of the developing brain (germinal matrix) rupture and bleed into the ventricles. This area is more susceptible to bleeding due to its underdeveloped blood vessels.
Intraventricular hemorrhage can lead to various complications, including accumulation of excess fluid in the brain (hydrocephalus), brain injury, paralysis and long-term developmental issues.
Grades of intraventricular hemorrhage
The severity of intraventricular hemorrhage is often categorized into four grades:
- Grade I: Bleeding is limited to a small amount in the germinal matrix.
- Grade II: Bleeding extends into the ventricles without causing significant dilation.
- Grade III: Ventricular dilation occurs due to the accumulation of blood.
- Grade IV: Severe bleeding with ventricular dilation, and it may also extend into the surrounding brain tissue.
Causes of intraventricular hemorrhage
There are several factors that can cause intraventricular hemorrhage. The most common causes include:
- Traumatic brain injury (TBI): Head trauma from accidents, falls or assaults can rupture blood vessels within the ventricles.
- Aneurysm rupture: Aneurysms are weak bulges in blood vessel walls that can burst, causing internal bleeding.
- Arteriovenous malformations (AVMs): These tangled connections between arteries and veins are prone to rupture.
- Hypertension: Uncontrolled high blood pressure can weaken blood vessels, increasing the risk of rupture.
- Cerebral amyloid angiopathy (CAA): This condition involves protein buildup in brain vessels, making them fragile and prone to bleeding.
- Brain tumors: Brain tumors can erode blood vessels or cause bleeding if they bleed themselves.
- Blood thinners: Medications like aspirin or warfarin can increase bleeding risk, especially in combination with other factors.
- Infections: Severe infections like meningitis can inflame and weaken blood vessels and lead to an intraventricular hemorrhage.
Symptoms of intraventricular hemorrhage
Symptoms of an intraventricular hemorrhage can vary depending on the severity of the bleeding and whether it is affecting other areas of the brain. In many cases, the symptoms may not be immediately apparent. Some immediately recognizable symptoms include:
- Loss of consciousness
- Seizures
- Coma
Early symptoms that may be subtle include:
- Headaches
- Nausea and vomiting
- Vision changes
- Weakness
- Difficulty thinking or speaking
Diagnosing and treating intraventricular hemorrhage
Getting a prompt diagnosis is essential to providing effective treatment and minimizing complications of an intraventricular hemorrhage and preserving optimal brain function.
To make a diagnosis, your doctor will review your medical history and perform a neurological exam to evaluate reflexes, balance and cognitive function.
Next, your doctor will use imaging testing such as a CT scan or an MRI to identify the severity and location of the bleed.
Intraventricular hemorrhage requires tailored treatment strategies based on the age group affected. There are differentiated approaches for premature infants and adults.
Advanced treatment options for infants
The primary focus is on stabilizing the infant and protecting their developing brain. This includes maintaining vital functions such as breathing and circulation, preventing infections and controlling seizures.
Diuretics may be used to reduce the fluid’s pressure and prevent hydrocephalus. Certain medications can also promote blood clotting and minimize further bleeding.
In severe cases, minimally invasive surgery may be necessary to remove blood clots and relieve pressure within the ventricles.
Advanced treatment options for adults
The first step is addressing the underlying condition that triggered the intraventricular hemorrhage, such as controlling high blood pressure, treating aneurysms, AVMs or stopping excessive bleeding due to medications.
Osmotic agents can be administered to draw fluid out of the brain and reduce intracranial pressure. Medications to control seizures and prevent blood clots may also be prescribed.
For severe cases with complications like hydrocephalus, surgical intervention may be necessary.
Prognosis and outcomes of intraventricular hemorrhage
The prognosis for individuals with intraventricular hemorrhage varies significantly. Outcomes are influenced by several factors, including severity, causation, timeliness of treatment, age and overall health.
Rehabilitation plays a crucial role in recovery and improving outcomes from an intraventricular hemorrhage. Physical therapy, speech therapy and occupational therapy can help manage long-term effects and support individuals in regaining lost skills and functionality.
Complications of intraventricular hemorrhage
Intraventricular hemorrhage can lead to various long-term complications, especially if the bleeding is severe or if it occurs in premature infants. The extent of complications can vary based on factors such as the grade of hemorrhage, timeliness of treatment and the presence of associated conditions.
Some potential long-term complications include:
- Hydrocephalus
- Neurological Impairments
- Cerebral palsy
- Intellectual disabilities
- Seizures
- Behavioral and emotional challenges
- Visual and hearing impairments
- Learning disabilities
It's important to note that not everyone who experiences intraventricular hemorrhage will develop these complications. Early detection, intervention and ongoing supportive care can play crucial roles in minimizing the impact of long-term complications.
Prevention of intraventricular hemorrhage
Preventing intraventricular hemorrhage involves addressing risk factors and implementing measures to reduce the likelihood of this condition, particularly in vulnerable populations such as premature infants.
Some strategies to prevent an intraventricular hemorrhage, include:
- Managing medical conditions like hypertension
- Avoiding head injuries
- Prenatal care for pregnant women at risk
- Make lifestyle changes and addressing maternal health issues
- Manage your blood pressure
- Wear protective head gear when riding a bicycle, motorcycle or at a job site
While these strategies can help reduce the risk of an intraventricular hemorrhage, it may not always be possible to prevent it entirely.
Are you at risk for stroke?
Most strokes are preventable and many of the risk factors are controllable. Our stroke risk quiz helps you estimate your chance of experiencing a stroke, find ways to minimize your risk and get an idea of what to do next based on your results.
Get care
We help you live well. And we’re here for you in person and online.