Spinal compression fracture
Request an appointmentSpinal compression fractures, often referred to as compression fractures, occur when more than one bone (vertebra) in the spine collapses or becomes compressed due to various factors such as injury, osteoporosis or other underlying medical conditions.
These fractures can happen in any part of the spine but are most common in the thoracic (middle back) and lumbar (lower back) regions. When left untreated, they can lead to back pain, limited mobility and deformity of the spine in severe cases.
Anatomy of the spine
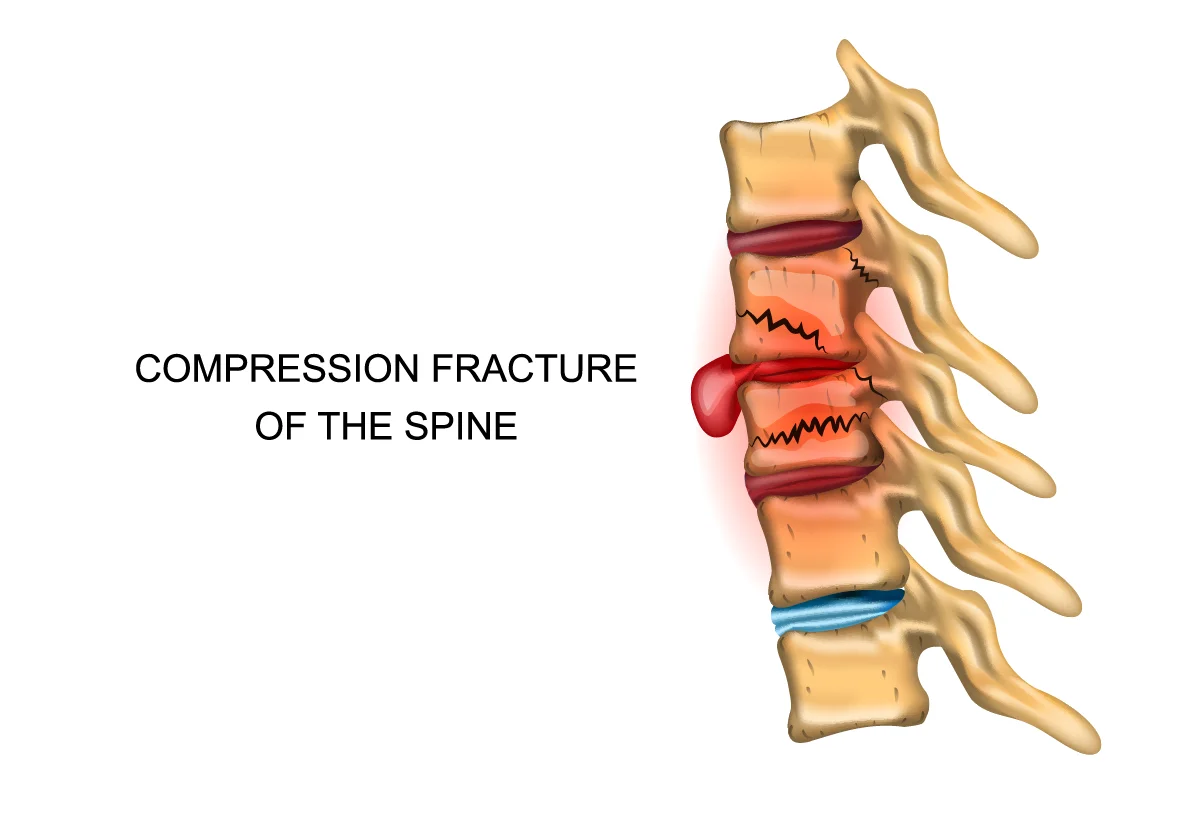
The above illustration shows a spinal compression fracture of two bones of the spine, commonly in the lower portion of the spine.
The spine serves as the central support structure of the human body, providing stability and flexibility. It also protects the spinal cord, a communication center for messages to and from the brain.
The spine consists of 33 vertebrae, stacked on top of one another like building blocks, forming five distinct regions:
- Cervical (neck)
- Thoracic
- Lumbar
- Sacral (hips)
- Coccygeal (tailbone)
These vertebrae are separated by intervertebral discs, which act as shock absorbers, cushioning the spine during exercise or movement.
Each vertebra comprises several key components, including the vertebral body that bears the weight of the body above it and the vertebral arch, which encloses the spinal canal.
Within the spinal canal lies the spinal cord. Surrounding the spinal cord are protective layers of tissue called meninges, which help safeguard against injury and trauma.
Protruding from the vertebral arch are bony processes that serve as attachment points for muscles, ligaments and tendons, contributing to the spine's stability and mobility.
Ligaments – bands of tough tissue –play a crucial role in connecting and stabilizing the vertebrae, while muscles surrounding the spine provide support and facilitate movement.
Causes of spinal compression fractures
Spinal compression fractures can occur due to many factors, ranging from traumatic injuries to underlying medical conditions. The most common cause is osteoporosis. Other common causes include:
- Osteoporosis: This condition weakens bones, making them more susceptible to fractures, even from minor trauma or everyday activities. Osteoporosis-related spinal compression fractures often occur in postmenopausal women and older adults.
- Trauma: High-impact accidents such as falls, car accidents or sports injuries can exert significant force on the spine, leading to spinal compression fractures.
- Spinal tumors: Cancerous or non-cancerous tumors that develop within or adjacent to the spine can weaken the vertebrae, increasing the risk of compression fractures.
- Vertebral fractures: Fractures in adjacent vertebrae can alter the biomechanics of the spine, placing increased stress on other vertebrae and potentially leading to a spinal compression fracture.
- Degenerative disc disease: Over time, the intervertebral discs between the vertebrae may degenerate, losing the ability to absorb shock and distribute pressure evenly along the spine.
- Spinal Infections: Infections such as osteomyelitis (infection of the bone) or discitis (infection of the intervertebral discs) can weaken vertebrae and predispose them to fractures.
- Metabolic conditions: Certain metabolic disorders, such as Paget's disease or hyperparathyroidism, can affect bone density and increase the likelihood of compression fractures.
- Medications: Prolonged use of corticosteroid medications, which are commonly prescribed for conditions such as asthma, arthritis or autoimmune disorders, can weaken bones and contribute to the development of compression fractures.
Individuals at risk should take proactive measures to maintain spinal health, including regular exercise, a healthy diet with plenty of calcium and vitamin D intake, and lifestyle modifications to minimize the risk of falls and trauma.
Symptoms of a spinal compression fracture
Spinal compression fractures can present with various symptoms, depending on the severity of the fracture and the underlying cause. Common symptoms may include:
- Back pain
- Limited mobility
- Height loss
- An abnormal curvature of the spine (kyphosis)
- Neurological symptoms such as numbness, tingling, weakness or loss of bowel or bladder control
- Radiating pain to other areas of the body, such as the abdomen, hips or legs
- Muscle spasms
- Difficulty breathing
Back pain that is persistent and localized is often the primary symptom of a spinal compression fracture. The pain may worsen with movement, standing, walking, or even with simple activities like coughing or sneezing.
It's important to seek medical attention if you experience any of these symptoms, especially if they're persistent or severe. Early diagnosis and treatment can help alleviate pain, prevent further complications and improve overall outcomes.
Is your back and neck pain cause for concern?
Back and neck pain can interrupt even the simplest things in life and can point to a serious problem. Our back and neck pain quiz evaluates your spine function, pain symptoms and risk factors and gives you an idea of what to do next based on your results.
Diagnosing spinal compression fractures
Diagnosing a spinal compression fracture typically involves a combination of testing methods. Your provider will begin by asking about your symptoms, including any recent trauma or activities that may have contributed to the onset of pain. They will also ask about any underlying medical conditions, such as osteoporosis or cancer.
During the physical examination, your provider will assess for tenderness, deformity and range of motion in the spine. They may also perform neurological tests to evaluate sensation, strength and reflexes in the arms and legs.
X-rays are typically the first imaging modality used to evaluate suspected spinal fractures. They can reveal changes in the alignment and structure of the vertebrae, such as compression or collapse.
MRI and CT scans are often used to provide detailed images of the spinal cord, nerve roots and surrounding soft tissues. They can help identify fractures, as well as detect any associated spinal cord or nerve compression.
Other testing, such as blood tests and a lumbar puncture may be used to look for underlying medical conditions.
In cases where osteoporosis is suspected as the underlying cause of the compression fracture, bone density testing (DEXA scan) may be performed to assess bone strength and density.
Spinal compression fracture treatment
Once a spinal compression fracture is diagnosed, your provider will develop an appropriate treatment plan based on the severity of the fracture, your symptoms and any underlying medical conditions.
Your provider may begin treatment for your spinal compression fracture with nonsurgical options, including rest and nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen or prescription opioid medications to manage pain.
Your provider may recommend a back brace or orthotic device to provide support to the spine and reduce pain during the healing process.
A structured physical therapy program may be included in your treatment plan to improve strength, flexibility and posture. Targeted exercises can help stabilize the spine, alleviate pain and prevent muscle atrophy. Strengthening the muscles surrounding the spine, particularly the abdominal and back muscles, can provide additional support and stability to the injured area.
Surgery is recommended if your fracture is severe or persistent. Your provider will refer you to an orthopedic surgeon. Surgical options may include:
- Vertebroplasty: Your surgeon injects a medical-grade substance called bone cement, which “glues” the spine in its proper position to reduce pain and bone deformity.
- Kyphoplasty: A balloon is inserted into the affected area to decompress your spine and allow you to regain lost height. Then your surgeon will inject bone cement to stabilize your vertebrae.
- Spinal fusion: An orthopedic surgeon will permanently adhere your vertebrae together in a fixed position.
Complications of a spinal compression fracture
It’s possible for spinal compression fractures to lead to various complications, ranging from acute symptoms to long-term issues. Some of the potential complications include:
- Chronic pain
- Loss of height
- Long-term limited mobility
- Spinal deformity, such as kyphosis (excessive rounding of the upper back) or scoliosis (sideways curvature of the spine)
- Weakness, numbness, tingling or loss of bowel or bladder control
- Increased risk of additional fractures
- Dependency on pain medications
Get care
We help you live well. And we’re here for you in person and online.