Rheumatoid arthritis
Find an ortho specialistRheumatoid arthritis (RA) is an autoimmune disease that causes inflammation in your joints. This inflammatory condition occurs when your immune system mistakes your joints as a threat and attacks them, causing painful swelling, primarily in your hands, wrists and knees.
Treating rheumatoid arthritis requires a multidiscipline approach with orthopedic specialists and rheumatologists. Your care team at Advocate Health Care will develop a treatment plan that helps you manage your symptoms and improve your quality of life.
Schedule an orthopedic appointment
From recent injuries to nagging aches and pains, our orthopedic specialists can help. Schedule an appointment in LiveWell, online or by phone.
What is rheumatoid arthritis?
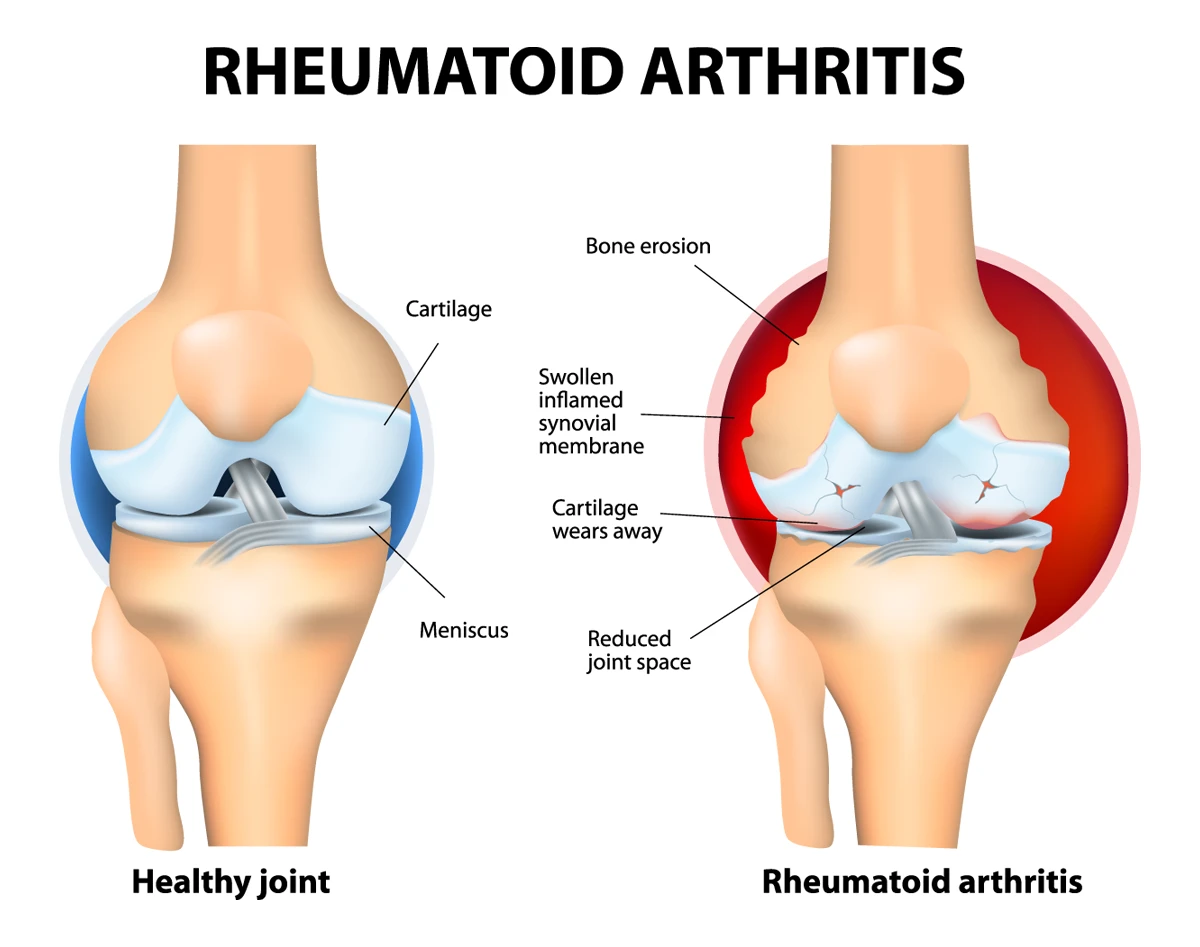
Rheumatoid arthritis causes damage to the synovial membrane in your joints, as seen on the right.
Rheumatoid arthritis is a chronic inflammatory disorder affecting your joints. This autoimmune disease occurs when your immune system mistakes your joints, primarily the synovial membrane (the protective layer around your joints), as a threat and begins to attack them.
This immune system response causes painful swelling, primarily in your hands, wrists and knees. Damage caused by rheumatoid arthritis can eventually result in bone erosion and joint deformity.
Rheumatoid arthritis vs. osteoarthritis
It's easy to confuse rheumatoid arthritis with osteoarthritis, but they are quite different. Osteoarthritis is a degenerative joint disease resulting from wear and tear, whereas rheumatoid arthritis is an autoimmune condition where your immune system attacks your joints.
While both cause joint pain and stiffness, rheumatoid arthritis often leads to more severe inflammation and can affect other parts of your body, including your skin, eyes, lungs and blood vessels.
Causes of rheumatoid arthritis
The exact cause of rheumatoid arthritis isn't known, but a combination of genetic and environmental factors is believed to be involved.
Certain genes may make you more susceptible to environmental factors, such as infections with certain viruses and bacteria, which may trigger the disease.
Smoking, obesity and exposure to environmental toxins like asbestos and silica also increase your risk.
Does rheumatoid arthritis get worse with age?
Rheumatoid arthritis can worsen with age. Without proper treatment, inflammation can lead to joint damage and loss of function over time. However, with early diagnosis and appropriate management, the progression can be significantly slowed, improving your quality of life.
How quickly does rheumatoid arthritis progress?
The progression of rheumatoid arthritis varies from person to person. Some experience a rapid onset of symptoms within a few weeks, while others have a slower, more gradual progression.
The disease can go through periods of flares (noticeable rheumatoid arthritis symptoms) and remissions (no symptoms), making the course unpredictable.
Diagnosing rheumatoid arthritis
Diagnosing rheumatoid arthritis involves a combination of medical history, physical exams, blood tests and imaging studies.
Blood tests can detect specific substances related to rheumatoid arthritis such as rheumatoid factor (RF) or anti-cyclic citrullinated peptide (anti-CCP) antibodies.
Imaging studies, such as X-rays, MRI or ultrasound, can help assess the extent of joint damage and inflammation.
Rheumatoid arthritis treatments and therapies
There is no cure for rheumatoid arthritis, but several treatments can help manage the symptoms and slow disease progression. Medications are typically the first line of treatment and may include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These medications help reduce pain and inflammation.
- Corticosteroids: Drugs like prednisone can reduce inflammation and suppress the immune system.
- Disease-modifying antirheumatic drugs (DMARDs): These drugs, such as methotrexate, can slow the progression of rheumatoid arthritis and save joints and other tissues from permanent damage.
- Immunosuppressive therapy: This is a drug regimen that reduces the body's immune system activity. It's mainly used to aid organ transplants, as the drugs help reduce the risk of the patient rejecting the new organ. However, it’s often used with autoimmune diseases as well.
- Biologic agents: These newer drugs can target parts of the immune system that trigger inflammation.
Orthopedic rehabilitation can also be beneficial in maintaining joint flexibility. In severe cases, surgical options like joint replacement may be considered to repair or replace damaged joints.
Lifestyle modifications for rheumatoid arthritis
Living with rheumatoid arthritis often requires lifestyle adjustments to manage symptoms and improve your quality of life. Here are some best practices:
- Exercise regularly: Low-impact activities like swimming or walking can improve joint health without adding stress. Strength training can help build muscles around your joints, providing better support.
- Maintain a healthy weight: Excess weight puts additional stress on your joints, especially your knees. Losing weight can alleviate some of the pain and improve mobility.
- Eat a balanced diet: A diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains and omega-3 fatty acids, can help reduce inflammation.
- Use assistive devices: Canes, splints or braces can help protect your joints and improve your mobility.
- Manage stress: Techniques like Pilates, yoga, meditation and deep breathing can help you cope with the stress and pain of living with rheumatoid arthritis.
Is that pain cause for concern?
Back, neck, hip or knee pain can cause severe discomfort and affect the way you live your life. Our pain quizzes evaluate your symptoms and risk factors and give you an idea of what to do next based on your results.
Get care
We help you live well. And we’re here for you in person and online.