REM sleep behavior disorder (RBD)
Find a doctorHave you ever wondered why you sometimes act out your dreams, which may include talking or physical movements? This phenomenon, known as REM sleep behavior disorder (RBD), can significantly impact your life and well-being.
REM sleep behavior disorder occurs when the muscle paralysis typical during REM sleep is incomplete, causing you to physically act out your dreams. This condition is closely linked with neurodegenerative diseases such as Alzheimer’s disease or multiple system atrophy and is more common in older adults.
If you or someone you know is experiencing RBD, Advocate Health Care’s Sleep Centers in Chicago are here to help. Our team of sleep specialists have access to the latest technology and sleep studies to help you overcome REM sleep behavior disorder.
Contact us to schedule a sleep disorder consultation near you.
What is REM sleep behavior disorder?
REM sleep behavior disorder is a condition where you act out your dreams during the REM stage of sleep. This stage is typically characterized by your muscles being temporarily paralyzed to prevent you from acting out your dreams.
In RBD, this paralysis is incomplete, leading to physical movements such as talking, shouting, punching or kicking. RBD is often associated with diseases such as Lewy body dementia and multiple system atrophy.
What is REM sleep
REM sleep, or rapid eye movement sleep, is a crucial phase of the sleep cycle where your brain is as active as it is when you’re awake, leading to vivid dreams. This stage is marked by rapid movements of the eyes, increased brain activity and temporary paralysis of most of your muscles. This is vital because it prevents you from physically acting out your dreams, thereby protecting you from potential harm.
During REM sleep, your brain processes and consolidates memories, regulates emotions and enhances learning and creativity. REM sleep typically begins 90 minutes after you fall asleep and recurs several times during the night, with each cycle getting progressively longer. A lack of adequate REM sleep can negatively affect your cognitive function, emotional stability and overall health.
The stages of sleep
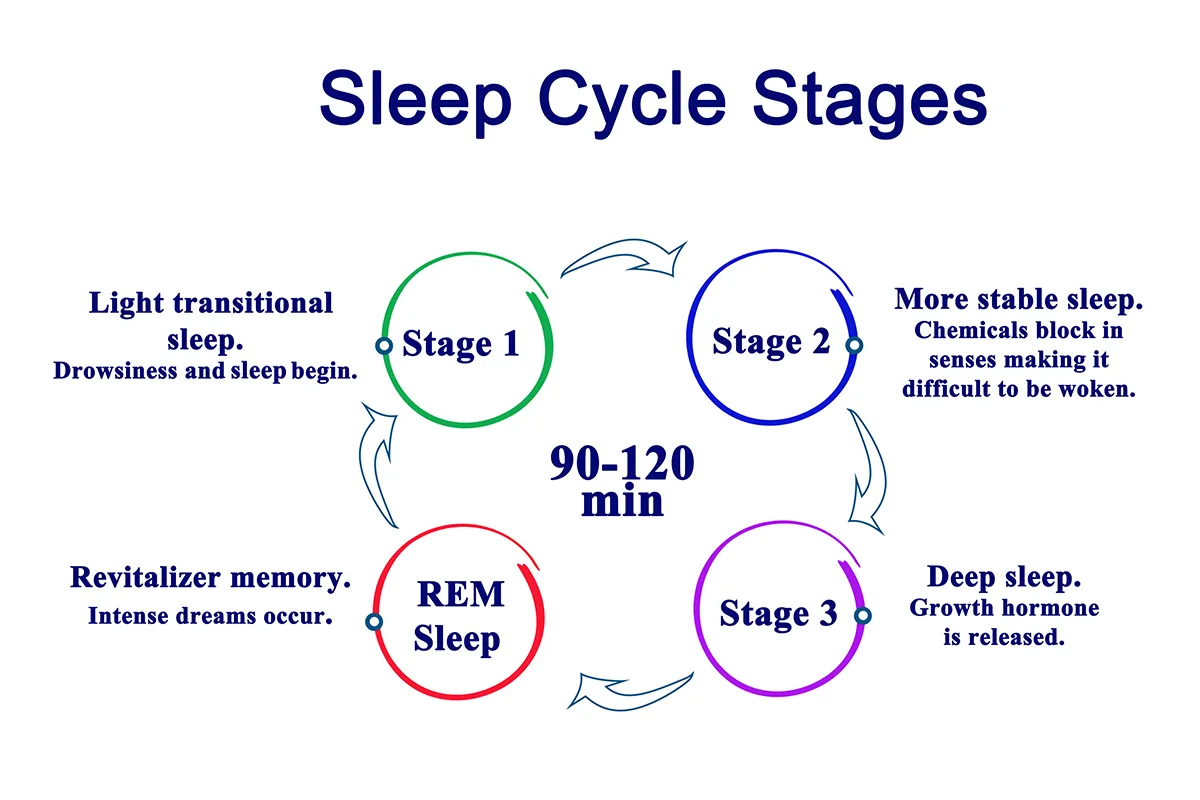
Your sleep cycle consists of several stages, including non-REM (NREM) and REM sleep. The cycle repeats multiple times throughout the night. Here is an overview of the stages of sleep:
- NREM stage 1: A light stage of sleep where you drift in and out of sleep. Your muscle activity slows down and your eyes move slowly.
- NREM stage 2: Your eye movements stop, and brain activity slows down during this stage. This is the largest portion of your sleep cycle.
- NREM stage 3: Also known as deep sleep, your body recovers from the day and repairs itself and grows new cells during this stage. It’s difficult to wake up from this stage.
- REM sleep stage: Your brain processes memories and what it learned during the day during this stage. You typically enter this stage 90 minutes after falling asleep. REM sleep is when most dreaming happens.
What are the causes of REM sleep behavior disorder?
The causes of REM sleep behavior disorder are not fully understood, but it’s frequently linked to neurodegenerative diseases. Certain medications and substance withdrawal, particularly from alcohol or sedatives, can also trigger RBD. In cases where no underlying condition is identified, it’s called idiopathic RBD.
What medications cause REM sleep behavior disorder?
Medications that affect REM sleep can also lead to RBD. Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), and other psychiatric medications have been associated with REM sleep disorder. Additionally, withdrawal from alcohol, sedatives or other substances can cause REM rebound, which happens when you get more REM sleep than normal due to withdrawal. It can look like RBD.
What are signs of REM sleep behavior disorder?
Signs of REM sleep behavior disorder include physically acting out dreams, vocalizations such as talking or shouting, and limb movements during sleep. These actions can be intense and may cause injury to yourself or your bed partner. If you notice these behaviors, it’s important to consult with a sleep medicine specialist for a proper treatment plan.
Sleep studies for REM sleep behavior disorder
A sleep study, or polysomnography, is essential for diagnosing RBD. This comprehensive test monitors brain waves, oxygen levels, heart rate, breathing, and eye and leg movements while you sleep. In some instances, at-home sleep studies are available.
The data collected helps confirm a REM behavior disorder diagnosis and excludes other sleep disorders. This information helps your sleep specialist develop an effective treatment plan for you.
How to stop REM sleep behavior disorder?
Treatment for REM sleep behavior disorder typically includes medications and lifestyle adjustments. Your doctor may prescribe Clonazepam, an anti-anxiety medication. This drug is often used to treat RBD. Melatonin supplements can also be beneficial.
Creating a safer sleep environment by removing hazardous objects and padding the area around your bed can help prevent injuries. Additionally, stress management and maintaining a regular sleep schedule can help improve REM sleep quality and reduce RBD episodes.
How to improve REM sleep
Enhancing your REM sleep can significantly improve your cognitive and emotional health. Here are some tips to improve sleep and help you improve the quality and duration of your REM sleep:
- Stick to a regular sleep schedule
- Develop a bedtime routine
- Reduce screen time before bed
- Manage stress and anxiety
- Avoid heavy meals and stimulants several hours before bedtime
- Ensure your bedroom is conducive to sleep by keeping it cool, dark and quiet
- Exercise every day
- Limit alcohol consumption
- Consider melatonin supplements
- Seek professional help if necessary
Get care
We help you live well. And we’re here for you in person and online.